The initiative permits primary care providers to prescribe buprenorphine, a medication for opioid addiction treatment, and nurses to offer patient care and support services.

The health department announced Monday the expansion of the Buprenorphine Nurse Care Manager Initiative, which provides buprenorphine, a medication for opioid addiction treatment, in health centers that serve people who are often uninsured or underinsured.
In the Buprenorphine Nurse Care Manager Initiative, primary care providers prescribe buprenorphine, and nurses offer additional patient care. The nurses screen and assess patients for treatment; manage medication to adjust dosing and track progress; support patient retention in care; facilitate insurance and payment issues, and refer them to supportive services such as housing and food benefits.
"Seeing the difference buprenorphine makes in our patients' lives is exciting; their physical and mental health improves," said Kate Kozeniewski, RN, Buprenorphine nurse coordinator at Bridgepoint Health. "Patients tell me that they feel better because they are repairing and growing relationships with friends, family and community."
In 2017, there were 1,441 confirmed overdose deaths; opioids were found in more than 80 percent of those deaths, according to the health department. The number of drug overdoses remains at epidemic levels as fentanyl, a potent opioid, continues to be present in the drug supply. Fentanyl has been found in heroin, cocaine, methamphetamine and ketamine, as well as in benzodiazepines and opioid painkillers acquired from non-pharmaceutical sources.
Treatment with buprenorphine or methadone is highly effective and can reduce the risk of overdose and death. Buprenorphine is an opioid partial agonist; like opioids, it produces effects such as euphoria or respiratory depression. With buprenorphine, however, these effects are weaker than those of full drugs such as heroin. Buprenorphine's opioid effects increase with each dose until at moderate doses they level off, even with further dose increases. This "ceiling effect" lowers the risk of misuse, dependency, and side effects. Also, because of buprenorphine's long-acting agent, many patients may not have to take it every day.
In 2016, approximately 13,600 New Yorkers received buprenorphine to treat their opioid addiction. Since the launch of the initiative in April 2017, nearly 350 patients have received buprenorphine treatment at 14 health centers citywide. The newly announced expansion will bring the initiative to an additional 12 health centers and is expected to offer buprenorphine treatment to over 5,000 patients.
The following health centers in Central and East Brooklyn are part of the Buprenorphine Nurse Care Manager Initiative:
- Bridgepoint Health/ Sterling Health Center, 803 Sterling Pl, Brooklyn, NY 11216
- Community Healthcare Network/ Williamsburg - Bushwick, 94-98 Manhattan Ave, Brooklyn, NY 11206
- HealthCare Choices at East New York, 179 Jamaica Ave, Brooklyn, NY 11207
The following newly funded health centers in Central and East Brooklyn will introduce buprenorphine treatment services for patients beginning in late 2018:
- Flatbush Family Health Centers at NYU Langone Health, 3414 Church Avenue, Brooklyn, NY 11203
- Interfaith Medical Center / Bishop Orris G. Walker, Jr. Health Center, 528 Prospect Pl, Brooklyn, NY 11238
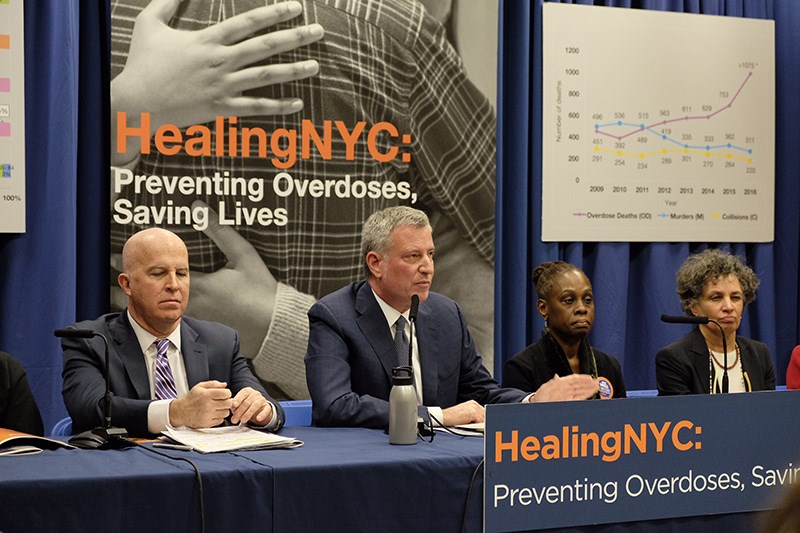
"In New York City, no one has to forgo lifesaving treatment for addiction. Buprenorphine is an evidence-based treatment option that can be administered by a nurse care manager and is available at an increased number of locations," said First Lady Chirlane McCray. "More locations for buprenorphine treatment will mean more second chances for New Yorkers."
Individuals seeking support or treatment for substance use issues for themselves or their loved ones can contact NYC Well by calling 1-888-NYC-WELL, texting "WELL" to 65173 or going to nyc.gov/nycwell. Free, confidential support is available at any hour of the day in over 200 languages.