For many breast cancer survivors, the healing process includes restorative care.
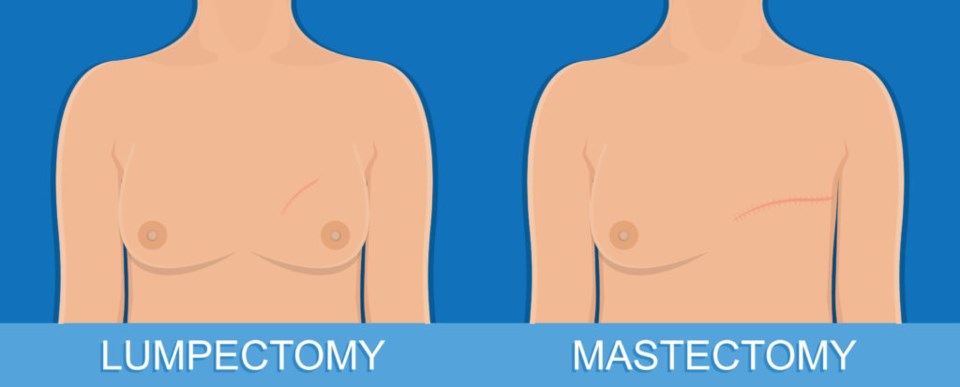
About 56% of women with stage III breast cancer undergo mastectomies — full removal of one or both breasts — according to the American Cancer Society. In earlier stages of cancer detection, almost 50% of women receive a procedure called a lumpectomy, otherwise known as breast-conserving surgery. Lumpectomies remove just the cancerous or abnormal tissue rather than the entire breast and are sometimes followed by radiation treatment.
Along with the surgeon performing their surgery, patients may be introduced to someone like Dr. Alyssa Golas, a plastic surgeon at New York University Langone Hospital in Brooklyn. Though she offers a spectrum of plastic surgery services, Golas specializes in breast reconstruction.

“I was really drawn to plastic surgery because we work all over the body head-to-toe," Golas said. "Every problem is different; every patient is different; every defect is different; every woman is different."
In honor of Breast Cancer Awareness Month, BK Reader talked with Golas about how she works with the breast surgeon to treat patients, the risks and benefits of reconstructive surgery and the importance of setting expectations.
BK Reader: What is the difference in terms of reconstruction options for a lumpectomy vs. a mastectomy?
Dr. Alyssa Golas: We only use implants after mastectomies, typically. For a lumpectomy, the way that we do it focuses on using your own tissue to camouflage the defects. So that can be rearranging some of the breast tissue from within the breast to camouflage the defects or doing something called fat grafting where we do liposuction somewhere else in the body and then inject that fat into the defect or into the breast to try to camouflage what was removed.
BKR: Let’s say a woman is preparing for a lumpectomy and is potentially interested in reconstructive surgery. What is the consultation process like?
AG: Ideally, we could do something on the same day as the lumpectomy.
What that means is I would talk with the breast surgeon about where the cancer is; ‘how big is the cancer; how much tissue do you think you're going to remove?’ And then after she does the lumpectomy, I would do some rearranging of the breast tissue to try to camouflage the procedure. That's called an oncoplastic closure. We can also do what's called a symmetrizing procedure on the other breast at the same time, and that can be a lift or what's also called a mastopexy or a reduction, just to make the two sides more even.
If you’re coming to me after you’ve had a lumpectomy, then it really is a patient-by-patient decision.
BKR: What are the risks of reconstructive surgery? What kind of questions should patients be asking when they consult with you or any other reconstructive surgeon?
AG: Any surgery risks bleeding, infection, healing problems, and then anytime you operate on the breast, there’s a chance of losing sensation in the nipple, losing part or all of the nipple, and then for women of childbearing age, there's always a chance of difficulty breastfeeding after pregnancy.
It's important to know about the recovery time and to talk about where their scars are going to be... And then I think they should really have an honest conversation about symmetry with the reconstructive surgeon.
BKR: You said there’s a ‘chance of difficulty' when it comes to breastfeeding. What does that mean?
AG: We don’t have great data about it. And the numbers we have are mostly after breast reduction. They say that about 60% of women are able to breastfeed to some extent after breast reduction, which includes some supplementation with formula. But a lot of women walking around on the street have difficulty breastfeeding anyway — it's so much more common than people talk about.
It’s just another one of those risks to be aware of. Another thing I would say is asymmetry and the differences between the two sides. I wouldn’t really call it a ‘risk’ but it’s something that patients should be prepared for as a possibility.
BKR: How much asymmetry are we talking about?
AG: I say ‘sisters and not twins,’ which I got from one of my teachers a long time ago. Our rib cages are different left and right; our shoulders; our collarbones, so I try to get them as close as I can, but there's no way to make everything totally, totally the same.
Especially for women who have big differences starting out, I can usually get them a whole lot closer than they were to start with, but symmetry in the human body is an impossibility.
BKR: What is the recovery time for a reconstructive procedure?
AG: If you're just having a lumpectomy alone, recovery from surgery is pretty fast, probably a couple of weeks. If we're doing other procedures on the breast I tell patients not to exercise or do anything strenuous for a month after surgery. Usually, by a month, people are really back to themselves.
BKR: Many people feel vulnerable in healthcare settings, where they’re exposed and reliant on others to take care of them. This is probably especially true for women who have battled breast cancer or had a scare. How do you offer reassurance and how have you learned as a doctor to improve your patient care?
AG: It's really important to listen to patients. Every patient has their own set of concerns and things that are important to them. And, I think one of the best things you can do for patients is just be honest. As long as they know that I'm always going to tell them the truth, that can be reassuring.




